For a while vitamin D was looking like a bona fide health elixir. It was recognized a century ago as the cure for rickets, a childhood disease that causes weak and deformed bones. Then, in the early 2000s, researchers began amassing a pile of studies suggesting that low vitamin D levels could be a factor in cancer, cardiovascular disease, dementia, depression, diabetes, autoimmune diseases, fractures, respiratory illnesses and Parkinson’s disease. It seemed reasonable to think that raising our levels of this simple vitamin—one that our bodies make when lit up by sunshine and that we can get more of from supplements—could cure practically whatever ailed us.
Thank you for reading this post, don't forget to subscribe!At least two books called The Vitamin D Cure were published, along with other books and news reports whose titles include words like “revolution” and “miracle.” There was also a growing concern that we weren’t getting enough of the vitamin. Good Morning America aired a segment that began with reporter Diane Sawyer declaring 100 million Americans were deficient. Her guest was Dr. Oz, who told viewers they could determine their vitamin D level with a simple blood test. Sunshine is the best way to get this vitamin, he said. But if that wasn’t enough, he advised cod liver oil or supplements.
Numerous celebrities and vitamin companies raised hopes that vitamin D could be a panacea, says JoAnn Manson, an endocrinologist and epidemiologist at Harvard Medical School and a lead investigator on some of the biggest vitamin D studies to date. Sales of supplements containing the vitamin soared, as did rates of vitamin D testing.
On supporting science journalism
If you’re enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
Then the bottom fell out. Although thousands of studies had linked low levels of vitamin D to an assortment of medical conditions, when scientists tried administering it as a means to prevent or treat those problems, the wonder supplement failed miserably. The notion that our lives would be better if we all just raised our vitamin D levels began to look like a fantasy. The idea that vitamin D deficiency was widespread also crumbled. It turned out that notions of what constitutes a deficiency were based on a dubious understanding to begin with. National population sampling showed that most people were already getting enough of the vitamin.
There’s no question that vitamin D plays an important role in health. It helps your body absorb and retain calcium and phosphorus; both are critical for building bone. But except for a few subsets of the population (such as breastfed infants and people with particular medical conditions), most people probably don’t need supplements.
The story of how vitamin D was discovered, rocketed to miracle status and then returned to Earth illustrates the sometimes jagged path of scientific discovery. It’s also a cautionary tale about the need to interpret scientific results with humility. Ultimately it’s about the self-correcting nature of science and how knowledge becomes honed over time.
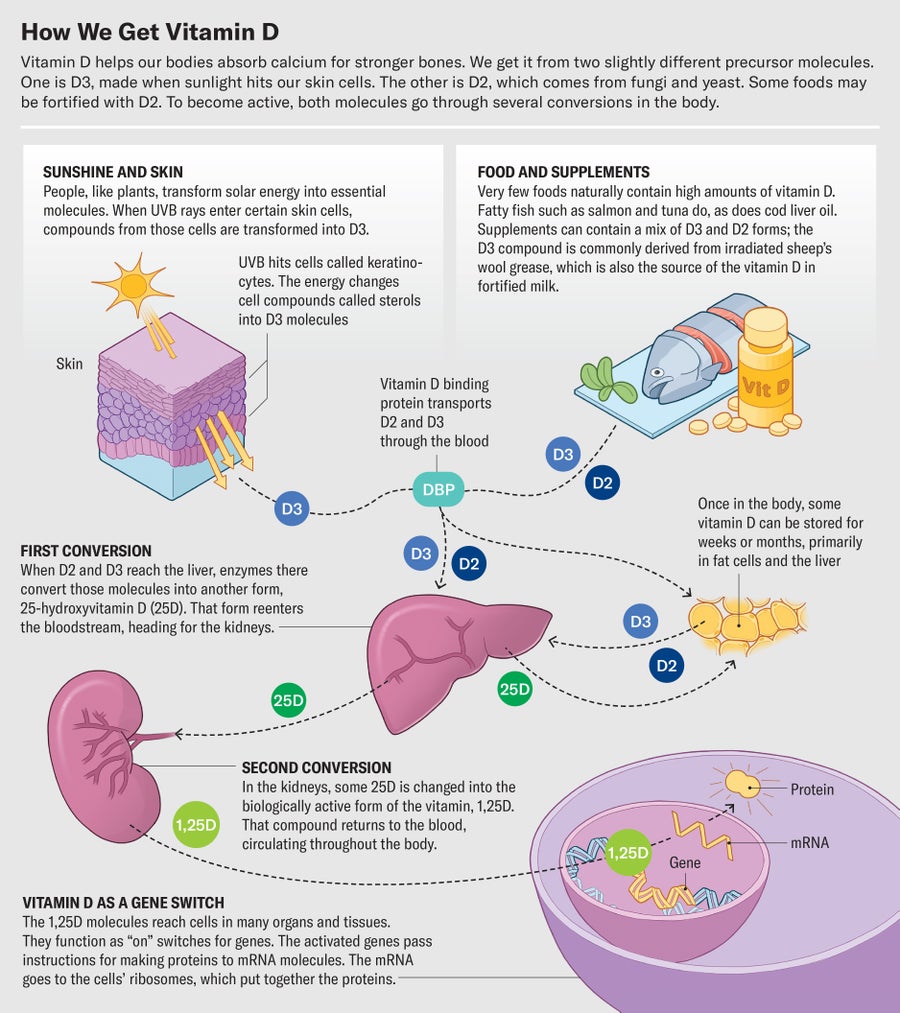
For much of human history, people got their vitamin D mostly from the sun. It turns out humans are a little bit like plants—we can turn ultraviolet light into something our bodies need in a process akin to photosynthesis.
When the high-energy rays of UV light—UVB—hit your skin, they start a chain reaction that converts a compound in your skin called a sterol into a vitamin D precursor. This molecule, after a few more steps, becomes a form of the vitamin that promotes calcium absorption from the gut and increases bone mineralization. Vitamin D also seems to bolster the immune system and tamp down inflammation. It does these things in part by influencing the production of inflammatory compounds and suppressing the buildup of proinflammatory cells. Researchers are studying whether vitamin D can prevent dangerous inflammatory reactions in people with COVID.
Producing vitamin D became increasingly difficult for human bodies during the Industrial Revolution, when smoke and soot darkened the skies and children spent more time in the shade of crowded cities, leading to an increase in rickets. By the late 1800s researchers had documented geographic differences in the prevalence of rickets that pointed to a possible link to sunlight.
In the 1920s Johns Hopkins University biochemist Elmer McCollum identified vitamin D in cod liver oil and gave it its name. German chemist Adolf Otto Reinhold Windaus won a Nobel Prize in 1928 for showing how the body made vitamin D from sunlight. Calling this previously unknown substance a vitamin gave it a sheen of beneficence. The term “vitamin” had been coined by Polish scientist Casimir Funk, who created the word by combining the terms “vita” (Latin for “life”) and “amine” (for amino acids, building blocks of life). The word created “an aura of safety and health,” says Catherine Price, author of Vitamania: How Vitamins Revolutionized the Way We Think about Food.
The practice of fortifying food with vitamin D began when McCollum’s former student Harry Steenbock, then at the University of Wisconsin–Madison, discovered that he could produce vitamin D in both rats and their feed by irradiating them with UV light. The rays hit sterol compounds, found in the cells of plants, animals and fungi, and start a conversion process. For instance, exposing chickens to UVB light boosts the vitamin D in their meat and egg yolks. Most of the vitamin D in modern supplements comes from irradiated lanolin, a grease derived from sheep’s wool. Steenbock also found that feeding dairy cows irradiated feed or mixing irradiated fat extract into milk raised D levels. Today fortified milk and other dairy products—which also use the lanolin-derived form of the vitamin—are some of the most common dietary sources.
In 1936 the Joseph Schlitz Brewing Company introduced “Sunshine Vitamin D” beer. The ads exclaimed that “beer is good for you—but SCHLITZ, with SUNSHINE Vitamin D, is extra good for you. Drink it daily—for health with enjoyment.” If it sounds antiquated, consider that in 2022 beer brand Corona launched Corona Sunbrew, a nonalcoholic beer fortified with vitamin D.
Beer is not, however, a health food. The “natural, evolutionarily appropriate way to get vitamin D is through synthesis in your skin,” says Anastassios Pittas, chief of the division of endocrinology, diabetes and metabolism at Tufts Medical Center. But that does not require getting a sunburn. It turns out that you don’t need high doses of sun to get sufficient vitamin D. A 2010 study calculated that between April and October, someone in Boston with 25 percent of their skin exposed would need between three and eight minutes of sunlight per day to get enough. Of course, in the winter it might be challenging to find even this amount of sun at some latitudes.
Fortunately, your body is equipped to deal with this kind of variation. Your liver and fat cells store vitamin D for future use, Pittas says. That means you don’t necessarily need a big dose every day. Your vitamin D cache generally lasts for about 10 to 12 weeks, so even if you don’t have a lot of daily D coming in via sunshine in the winter, Pittas says, you could still have enough circulating from your liver to maintain adequate calcium and phosphorus levels. It’s natural to have a winter dip, he says, but that is worrisome only if you’re already running low on vitamin D.
Interest in getting extra vitamin D took off when studies suggested it might lower the risk of heart disease, cancer, diabetes, and a range of other conditions.
The problem is that this evidence came mostly from observational studies, a type of analysis that can’t show cause and effect and that might produce misleading results, Manson says. These observational studies looked for associations between vitamin D levels and a particular health issue or compared vitamin D status among people with a condition and those without. For instance, an offshoot of the Framingham Heart Study published in 2008 followed more than 1,700 people without prior cardiovascular disease over about five years and found that people with low vitamin D levels had a higher risk of developing heart disease. The results generated a lot of excitement and hype around vitamin D, Manson says.
Diabetes, too, seemed to track with D levels. A study published in 2010 followed close to 6,100 people in Tromsø, Norway, over a period of 11 years. Their incidence of type 2 diabetes showed an inverse relation with blood levels of vitamin D before their body mass was taken into account: higher D levels were correlated with fewer cases of diabetes. Similarly, a 2011 study of more than 6,500 people in Australia found that the risk of developing diabetes over the course of five years was lowest for the participants with the highest D levels.
All these observational studies have a fundamental weakness: they can identify a co-occurrence between vitamin D and a disease, but they can’t prove there is a cause-and-effect relation—or, if there is one, they can’t identify in which direction it might go. Think of it this way: there’s a strong link between someone’s wealth and the price of their car, but that doesn’t mean buying an expensive vehicle will make you rich.
“Just because you see an association, that doesn’t mean that, okay, if we fix the serum vitamin D level, that’s going to fix the problem,” says physician Leila Kahwati, associate director of the Research Triangle Institute–University of North Carolina Evidence-based Practice Center. There might be other factors at play. For instance, people who take vitamin D supplements may be more health conscious and do other things that protect them from disease, and people who are already in poor health probably spend less time outdoors getting vitamin D from sunlight.
For these reasons, randomized controlled trials, in which researchers recruit a group of participants and then assign them to receive different treatments (or a placebo), are considered the strongest kind of medical evidence, says physician Jodi Segal, associate director of the Center for Health Services and Outcomes Research at Johns Hopkins University’s school of public health. A randomized design makes it much more likely that any differences between the study and placebo groups are caused by the intervention rather than by some other variable.
In 2009 Manson and her team embarked on the world’s largest and most far-reaching randomized vitamin D trial, called VITAL. The study followed nearly 26,000 generally healthy adults, randomized to receive either 2,000 international units (IU) of vitamin D or a placebo, for an average of 5.3 years. The volunteers were almost evenly split between men and women, and 20 percent of the participants were Black. The study was designed to look at whether vitamin D supplements could prevent cancer or cardiovascular disease.
The results came as a shock. Not only did vitamin D not make a dent in rates of cancer or heart disease, but the trial also found that vitamin D did not prevent falls, improve cognitive function, reduce atrial fibrillation, change body composition, reduce migraine frequency, improve stroke outcomes, decrease age-related macular degeneration, reduce knee pain or even reduce the risk of bone fractures. The finding about fractures “was a real surprise to many people,” Manson says.
Extra vitamin D also didn’t lower diabetes risk. In a trial published in 2019 in the New England Journal of Medicine, Pittas and his colleagues randomized more than 2,400 people at risk for diabetes to take either 4,000 IU of vitamin D or a placebo daily. After two and a half years, a similar number of people in each group went on to develop the disease.
The Vitamin D Assessment Study (ViDA) recruited 5,110 volunteers ages 50 to 84 in New Zealand and randomized them to get either a placebo or 200,000 IU of vitamin D per month—a huge dose much higher than the recommended daily allowance. The study found that levels made no difference in cardiovascular disease, acute respiratory infections, nonspinal fractures, falls and all types of cancer. Other trials found that vitamin D supplementation did not reduce mortality rates or the risk of invasive cancer. These results, along with others coming out of VITAL, led to growing skepticism about vitamin D by around 2020, says Clifford Rosen, an endocrinologist at the Maine Medicine Center’s Research Institute.
The ViDA trial did find some modest supplement benefits in people who had started the study with a vitamin D deficiency. But what exactly does “deficiency” mean?
It does not mean what many doctors think it does, apparently. The widespread notion that much of America is walking around deficient in vitamin D came from what Manson calls a “misinterpretation and misapplication” of the normal levels for vitamin D set by the Institute of Medicine (IOM, now known as the National Academy of Medicine) more than a decade ago.
Here’s what happened. In 2011 the IOM convened an expert committee to conduct a thorough analysis of all existing studies on vitamin D and health. Based on this evidence, the committee concluded that the bone-strengthening benefits of vitamin D plateau when blood levels (as measured by a standard vitamin D blood test) reach 12 to 16 nanograms per milliliter. They also found that there were no benefits to having levels above 20 ng/ml. So they set that as the ceiling for their recommendations while noting that the majority of the population is just fine at 16 ng/ml.
According to measurements of vitamin D levels in the general U.S. population collected through the National Health and Nutrition Examination Survey, most people had levels of 20 ng/ml or more in 2011. Levels have actually risen since then, meaning that most people are well within the medical recommendations, says Rosen, who served on the IOM committee.
So where did the idea of mass deficiency come from? First off, 20 ng/ml was erroneously interpreted by some health-care workers as the bare minimum, instead of a level marking good amounts for most people. Recall the IOM found that 16 ng/ml was satisfactory. The implication of the misreading was that people needed more than 20 ng/ml for good bone health, Manson says.
But some of the confusion stems from a second set of guidelines that another medical group, the Endocrine Society, put out around the same time as the IOM standards. Whereas the institute made recommendations for healthy populations, the society’s guidelines were aimed at clinicians, particularly those caring for patients at risk for vitamin D deficiency. The makers of these guidelines looked at much of the same evidence that the institute committee reviewed, but they concluded that anything under 20 ng/ml represented “deficiency,” and they labeled vitamin D levels of 21 to 29 ng/ml as something they called “insufficiency.”
The terms “insufficiency” and “deficiency” have created “a tremendous amount of confusion,” says Christopher McCartney, an endocrinologist and clinical research specialist at the University of Virginia School of Medicine. He adds that the Endocrine Society guidelines have been largely taken to mean that everyone needs vitamin D levels of 30 ng/ml or more.
The IOM guidelines don’t support that conclusion, and in 2012 the institute committee published a rebuttal paper, “IOM Committee Members Respond to Endocrine Society Vitamin D Guideline.” It contended that aspects of the society’s guidelines, including the definition of insufficiency, were not well supported by evidence. For instance, the society’s guidelines used a 2003 study of only 34 people to support its contention that vitamin D levels above 30 ng/ml are better for calcium absorption. At the same time the society’s committee ignored a study of more than 300 people that found that calcium absorption pretty much maxes out at vitamin D levels of 8 ng/ml.
Michael Holick was the lead author of the Endocrine Society guidelines. An endocrinologist at Boston University’s medical school, Holick says that the insufficiency standard is justified by an observational study from 2010. It found that about a quarter of the otherwise healthy adult males had evidence of osteomalacia, a bone-softening condition linked to low vitamin D levels. The study didn’t find bone problems in people above 30 ng/ml; hence Holick’s contention that 30 was the minimum.
The Endocrine Society is currently in the process of updating its guidelines, with McCartney serving as its methodologist. He says that the new guidelines will focus on randomized trials, not observational ones, and they’ll be careful to call out the evidence gaps that remain.
The committee is also taking care to avoid outside influence. “Our conflict-of-interest policy is much more transparent and rigorous than I think it has been in the past,” McCartney says. Holick, who ran the original guideline-writing group, advocates large doses of vitamin D supplements. Although there is no evidence that his judgments were affected by commercial ties, Holick has received at least $100,000 from various companies involved in making vitamin D supplements and tests, according to a 2018 investigation by Kaiser Health News (now KFF Health News) and the New York Times. McCartney says that, in part, concerns raised about Holick prompted the Endocrine Society to pay extra attention to ethics.
Holick made a name for himself espousing the health-promoting powers of vitamin D and wrote a book called The Vitamin D Solution: A 3-Step Strategy to Cure Our Most Common Health Problems. He takes 6,000 IU daily and advises his patients to take a minimum of 2,000 to 3,000 IU per day. For comparison, the 2011 IOM report calculated that the average person’s daily requirement is 400 IU.
Holick told Scientific American that it is “not true” that he has conflicts of interest. He acknowledged receiving industry money but said most of the money had “nothing to do with vitamin D” and was instead “associated with me talking about a new drug coming on the market,” for patients with chronic hypoparathyroidism.
Still, some in the field see Holick’s evangelism for vitamin D as conflicting with his role working on the Endocrine Society guidelines. Rosen says that the guidelines “were driven by Mike. He was the chair of the committee.” Rosen trained with Holick and considers him a friend. “He’s a good guy,” Rosen says. But “just because you hypothesize something doesn’t mean you have to stick with it…. Michael went to extremes to show that vitamin D had something to do with chronic diseases.”
Much of the information put out by companies offering direct-to-consumer testing still claims that anything under 30 ng/ml is low. Athlete Blood Test, for instance, markets blood tests to active people and encourages them to aim for a level of at least 50 ng/ml. While working on this story, I had my vitamin D checked by another testing company, and the laboratory results came back with reference ranges of 30 to 100 ng/ml, implying that anything under 30 was not enough. The lab explanation did note that the IOM’s cutoff was 20. (My number was 32.8 ng/ml, which suggests that sunshine really can help—I never take supplements, but I exercise daily outdoors.)
More than 10 million vitamin D tests are done annually in the U.S., despite the fact that these tests are not recommended by major medical organizations such as the Endocrine Society, the National Academy of Medicine and the U.S. Preventive Services Task Force. Three medical societies have endorsed a recommendation to “not order population-based screening for vitamin D” from Choosing Wisely, an initiative to reduce wasteful medical practices.
Yet the testing goes on. A study published in 2020 examined medical records from a large regional health system in Virginia and found that about 10 percent of the system’s patients were tested for D levels, although many of the tests were not indicated by the patients’ health conditions. Supporting the idea of the tests being unneeded, 75 percent of the results came back as normal, says study author Michelle Rockwell, an assistant professor of family and community medicine at the Virginia Polytechnic Institute and State University. Furthermore, some of the test results categorized as abnormal may have been considered just fine by the IOM standards; the study used a higher reference range of 30 to 99.9 ng/ml.
Given the VITAL trial’s large size and wide scope, many vitamin D researchers hoped it would put many of the purported benefits of vitamin D supplements to rest. “But there’s a religiosity around vitamin D,” Rosen says. Rosen wrote an editorial in the New England Journal of Medicine saying most people can stop taking vitamin D supplements and that the large VITAL study was a “decisive verdict.” Even then, he says, he got pushback from colleagues who refused to believe that vitamin D wasn’t the panacea they had come to believe. “The evidence is out there,” he says. “People don’t want to pay attention to it.”
Although most people don’t need supplements, there are exceptions. Breast milk does not contain enough vitamin D for infants, so the American Academy of Pediatrics recommends that babies who are breastfed (partially or exclusively) be supplemented with 400 IU a day of vitamin D beginning in the first few days of life to promote stronger bones. In addition, the academy says all infants and children who consume less than 32 ounces of vitamin D–fortified formula or milk per day should also get supplements of 400 IU. Crohn’s disease, cystic fibrosis, celiac disease, and certain liver and kidney conditions can cause vitamin D deficiency, so people with these illnesses might also need supplements. People who are hospitalized or who have had gastric bypass surgery may also become deficient.
Typical tests may, however, overestimate vitamin D problems in some people of African ancestry. The standard test measures circulating blood levels of a vitamin D precursor, 25-hydroxyvitamin D, that is bound to a particular protein. A 2013 New England Journal of Medicine study found that some people have gene variants that allow circulation of more of the unbound precursor form and less of the bound one. So by focusing on the bound version, the test underestimates total vitamin D availability. The study, which involved more than 2,000 people, found that those who were Black had lower vitamin D levels than white participants according to the standard blood test. Yet those Black people had strong bones and good calcium levels.
Manson is quick to caution that more isn’t necessarily better when it comes to vitamin D. “Vitamin D is essential to good health, but we require only small to moderate amounts,” she says. She doesn’t dissuade people from taking supplements of up to 2,000 IU per day, but she doesn’t recommend higher levels because some studies have found that excess vitamin D can increase the risk of dangerous falls—researchers speculate that intermittent high doses affect the central nervous system, which could impair balance. And whether you’re taking supplements or not, you are probably getting supplemental vitamin D if you consume dairy products, breakfast cereal, plant milks, or other fortified foods, says Price, author of Vitamania.

Despite the disappointing trials on vitamin D, it’s not time to dismiss the vitamin completely, Manson says. There’s still plenty more to understand. For instance, the VITAL trial showed that among slender or normal-weight people, defined as having body mass indexes of 25 or less, vitamin D supplements appeared to lower the incidence of cancer, cancer deaths and autoimmune disease. This protective effect did not show up among heavier people with higher body masses. Manson cautions that these numbers need to be verified by further work because they are from a smaller subanalysis of the main study. But it’s possible that excess body fat may somehow hamper the effectiveness of vitamin D. Obesity itself is a risk factor for both cancer and autoimmune disease, so it’s likely that any connection is complex.
Pittas remains convinced that for people at high risk for diabetes, vitamin D can play a role in prevention. His earlier trial did hint that people who received supplemental vitamin D were less likely to develop diabetes: 24.4 percent of them got the disease, versus 26.9 percent of the placebo group. That difference alone was too small to be statistically significant. But when he pooled the results with those of two other randomized trials, he found a modest but consistent benefit of about a 3 percent reduction in diabetes risk over three years.
There are some positive signs for treating COVID, too. Clinical and lab studies have shown that vitamin D has a positive effect on the immune system and can tamp down inflammation. “We saw this in our VITAL trial,” Manson says. Holick adds that vitamin D can help downregulate so-called cytokine storms, immune system overreactions that have provoked life-threatening respiratory problems in some COVID patients.
Manson’s research group has two randomized trials currently underway to test whether vitamin D can help with COVID. One is investigating whether high-dose vitamin D can reduce the chances of getting the extended and debilitating ailment of long COVID. The other trial is looking at whether 1,000 IU of vitamin D per day can reduce the risk of that illness or overall symptom severity. Manson hopes to finish analyzing the data in 2024.
Vitamins hold a certain allure. They’re cheap, they’re relatively safe, and there’s a sense, emphasized by marketers, that they’re “natural” and therefore somehow better than drugs, Rosen says. “There’s this magical thinking that vitamins improve health, and some people do feel better” when taking them, he says, pointing to the placebo effect as a potential contributor.
The ups and downs of vitamin D offer a lesson in humility. The relation between the vitamin and disease is far more complicated and nuanced than it first seemed and a reminder that scientific understanding is always evolving.