September 4, 2024
Thank you for reading this post, don't forget to subscribe!4 min read
A small study of transgender men taking testosterone revealed changes in immune pathways involved in responding to viruses and inflammation
By Tanya Lewis
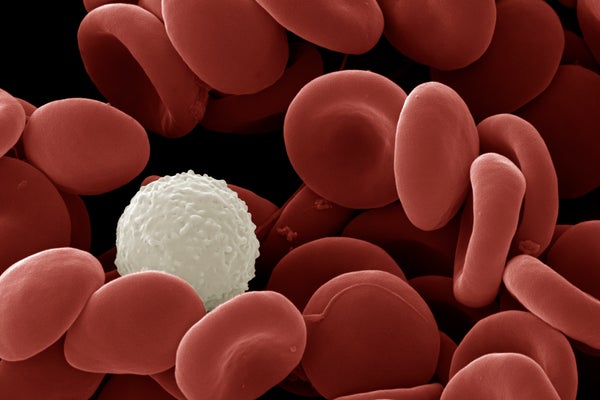
A recent study found that trans men taking testosterone had white blood cell changes that resembled cis men’s immune system activity.
David Spears FRPS FRMS/Getty Images
The immune systems of men and women are known to display key differences. Men are, broadly speaking, more vulnerable to viral infections such as COVID and influenza. Women mount a stronger response to viruses yet are more prone to autoimmune diseases, such as lupus. But the extent to which these differences arise from genetics, hormones or other factors is not well understood.
New research, published on Wednesday in Nature, offers some clues. Scientists in Sweden studied a small group of transgender men who were assigned female at birth and were taking testosterone as part of gender-affirming care. The researchers found the participants underwent changes in two distinct immune cell pathways involved in the response to viral infection and in inflammation.
“This study supports that testosterone impedes and attenuates these antiviral responses [known as] interferon responses while promoting these more inflammatory responses,” says Dawn Newcomb, an assistant professor of medicine at Vanderbilt University Medical Center, who studies the role of sex hormones in immune function but was not involved in the new paper. “These results fit very nicely with what we’ve seen previously in male and female cells from cis individuals.” (The term cisgender, or cis, means having a gender that corresponds to the sex one was assigned at birth.)
On supporting science journalism
If you’re enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
The study involved 23 transgender men between the ages of 18 and 37 while they underwent testosterone therapy. The researchers took blood samples from the participants before they began the hormone treatment and did so again three and 12 months afterward to look at changes in various immune cells and signaling proteins.
Within three months, most of the transgender men’s testosterone levels entered the typical range for cisgender men while their estradiol (the most potent form of estrogen that is made in the body) and progesterone levels decreased. Twelve months after starting hormone therapy, the participants showed a decrease in an immune response involving a protein called type I interferon, which the body uses to fight off viral infections. At the same time, they showed an increase in a signaling pathway that involves tumor necrosis factor (TNF), which is typically employed in fighting bacterial infections through inflammation. While not identical, these patterns somewhat resembled the immune activity seen in cisgender men.
While this is just one study, the results may have implications for the health of transgender men taking masculinizing hormone therapy. “We can’t say that these individuals are now more susceptible to any infection, and so on, but what we can say is that their immune profiles do alter or change in a way that is more similar to [cisgender] men,” says study co-author Petter Brodin, a professor of pediatric immunology at the Karolinska Institute in Stockholm.
To determine how much of the effect was linked to increased testosterone versus decreased estradiol, the researchers also took blood from healthy, cisgender female donors and exposed it to either testosterone or an estrogen blocker. They then measured the resulting immune changes and found that testosterone appeared to be directly involved in the TNF response. The type I interferon response was also affected by testosterone, but previous studies suggest estrogen may also play a role.
Newcomb notes that the study’s small number of participants is a limitation. “I think it’s important to understand [that sex hormones are] likely one mechanism—not the only mechanism—at play,” she adds. Genetics and epigenetics (modifications in gene activity) likely also affect immune development.
Brodin would like to see better monitoring of all patients receiving hormone therapy, whether for gender-affirming care or other reasons, such as estrogen or testosterone supplementation in cisgender men and women. “We should just urge caution for people taking hormone therapies for any purpose,” he says, “and make sure that we follow up to see that there are no health consequences that we don’t intend.”
Study co-author Nils Landegren, a physician and an assistant professor at Uppsala University in Sweden, whose research focuses on immunity, agrees that further studies are needed. “To be drawing conclusions on the risk for these individuals, we need to collect information about actual disease outcomes from these individuals. We will need much larger numbers and longer follow-up.” Landegren is now leading a study of transgender women who are taking female sex hormones that seeks to understand how that type of treatment may affect immune function.
So why do sex-based differences in immune function exist in the first place? One possible answer has to do with the fact that the female body invests a lot of resources in reproduction and pregnancy. Women may have evolved a stronger antiviral immune response to protect fetuses from infection, but they can’t produce too strong an inflammatory response, or it could harm a fetus. In addition, high levels of TNF have been linked to embryo implantation failure and pregnancy loss. By contrast, the male body has a much smaller role in reproduction and may prioritize muscle growth, which involves high levels of TNF.
“Our immune systems and how they are shaped over evolutionary time is this balance between surviving infections and the risk of autoimmunity,” Landegren says. “It’s fascinating to see how this balance is differently set in women and men.”

