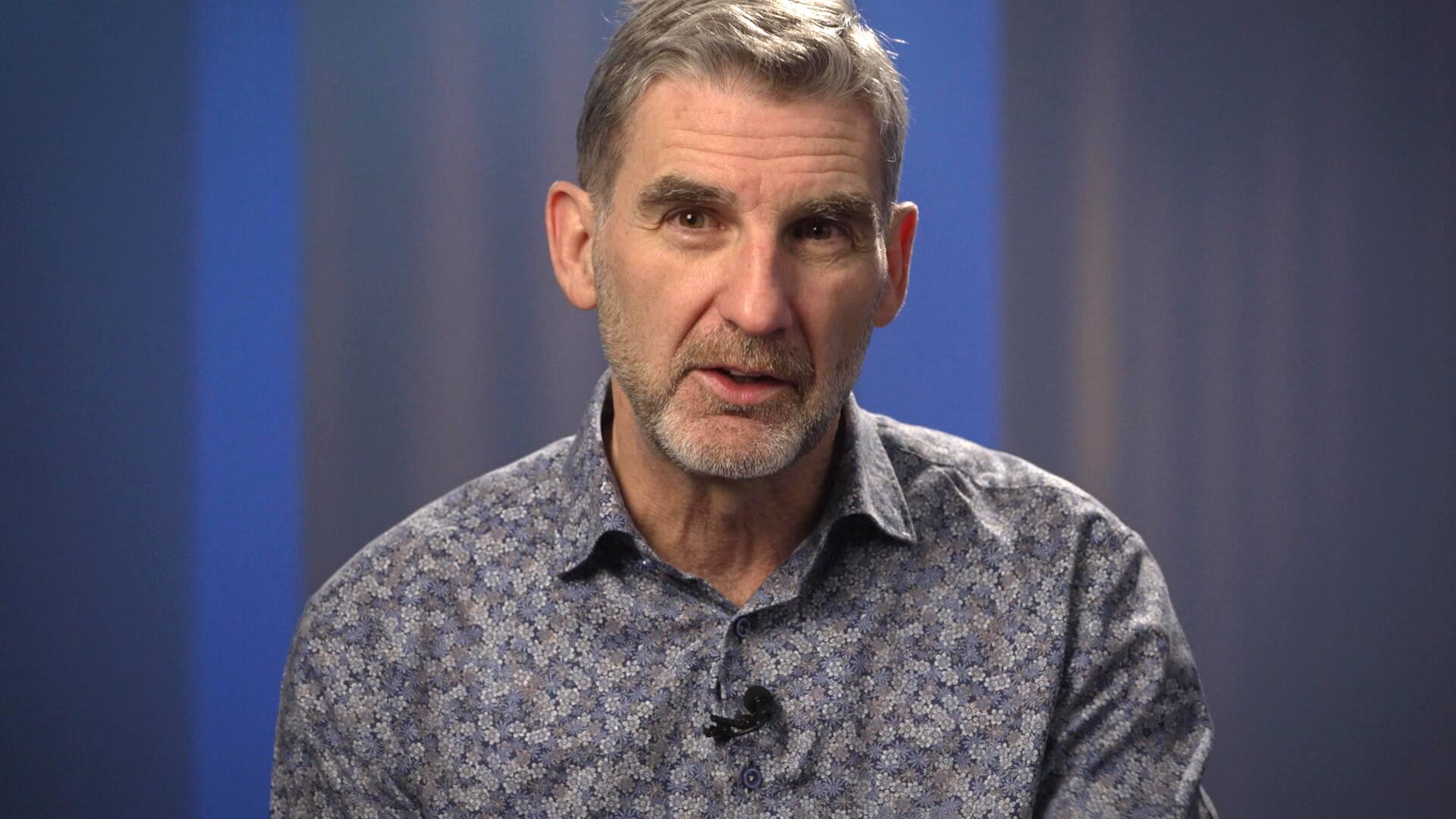
CBC journalist Harry Forestell applied his journalistic expertise to learn more about the highly specialized treatment he received to treat Parkinson’s disease.
Thank you for reading this post, don't forget to subscribe!
This First Person article is written by Harry Forestell, host of CBC News New Brunswick at Six, who draws upon his experiences with Parkinson’s disease.
My latest party trick is a real attention grabber.
It’s a vivid illustration of the before and after effects of my recent treatment for Parkinson’s disease. Proof of just how much a little poking around in the brain can achieve.
The treatment is called deep brain stimulation (DBS). It involves implanting thin electrodes into the brain where they emit tiny electrical pulses. Those pulses, applied continuously to just the right section of grey matter, stimulate centres in the brain that control signals sent to your muscles. In the basal ganglia, the engine house of the brain, signals are sent to the body ordering everything from speaking, to swallowing, to walking and touching. When those signals don’t get through, or when the instructions get scrambled, the body’s reaction can be cruel. Hands tremble uncontrollably, legs shake, walking becomes increasingly difficult, even swallowing is a challenge.
These are all early symptoms of Parkinson’s disease and the list is by no means exhaustive.
More than 84,000 Canadians suffer from symptoms of Parkinson’s disease. From 2011 to 2031, the number of Parkinson’s cases in Canada is expected to double.
Parkinson’s is considered a chronic but not fatal disease. As neurologists will often explain, you will die with Parkinson’s, not from Parkinson’s. While true, it doesn’t really capture the creeping, insidious progress of the disease as it deprives victims of the ability to control their own bodies.
Medical stories like this have always been a source of fascination for me. I worked for several years as a medicine and science reporter, covering stories that included the panic over mad cow disease in the U.K. I produced radio features on brain development and decay.
WATCH | How deep brain stimulation can help overcome debilitating effects of Parkinson’s:
See the almost instantaneous effects of deep brain stimulation for Parkinson’s disease treatment
Harry Forestell shows how DBS therapy can work in daily life — and demonstrates what happens when he turns it off.
Little did I know that I eventually would be reporting on my own brain malady.
A shock of a diagnosis, and a relief
The day my diagnosis of Parkinson’s disease was officially confirmed came as much of a relief as a shock.
It was 2015 and for the previous two years, my wife Jenny and I had been careering back and forth between hope and despair. My Fredericton neurologist, Dr. Eva Pniak, a patient and persevering soul, suspected Parkinson’s, but suggested the problems I experienced walking and with my tremoring hands could also be explained by a modestly more benign condition called essential tremor.

She referred me to a specialist in Toronto where the diagnosis was conclusive.
At 53, I had Parkinson’s.
From leaping out of a tree to dancing the tango, very little happens in the body without first being ordered by the basal ganglia. Those orders are sent at the speed of light through nerve networks with the help of a neurotransmitter called dopamine. It is the as-yet unexplained decline in the brain’s dopamine-producing cells that leads to movement disorders like Parkinson’s.
It’s a simple equation: no dopamine, no movement.
With Parkinson’s, those dopamine cells start quietly dying off years before symptoms first appear. Scientists aren’t certain why this happens, or why the process cannot be stopped or slowed.
Doctors can replace some of the lost dopamine with a medication called levodopa, but it causes a side effect known as dyskinesia — sudden uncontrolled muscle movements in the arms and upper body that create a writhing, torquing motion. As doctors increase doses of levodopa to stave off Parkinson’s tremors, dyskinesia increases.
The payoff is in quality of life for patients
Neurologists have been experimenting with DBS to treat Parkinson’s and other movement disorders for nearly 40 years. In 1997, the U.S.-based Food and Drug Administration approved DBS to treat Parkinson’s disease.
The procedure has been available in Canada since 2012. Fewer than 400 patients a year undergo DBS in Canada.
Why not more? The simple reason is that it is a treatment involving intricate brain surgery by highly specialized surgical teams and requiring considerable aftercare.
Dr. Tony Lang leads the Toronto Western Hospital Movement Disorders Clinic, a world-leading centre for deep brain stimulation.
“The surgical expertise is extremely important,” he said.

“You have to have a surgeon that knows how to do the procedure and knows how to put the electrodes in the right spot. But then after the surgery, you need an expertise in doing all of the programming and adjusting the stimulators and also adjusting the medication doses which typically change after the operation,” he said.
“So it’s a very complicated procedure that requires a team and it’s the neurologist and the nurses after the surgery that are doing a great deal of the work in optimizing the responses.”
It is a procedure, Lang points out, that requires support from provincial governments. The payoff is a treatment that can offer major improvements in quality of life for Parkinson’s patients.
“The Ontario government has appreciated the importance,” said Lang, adding he feels lucky to have a team of expert neurosurgeons, neurologists, nurses and others to support patients.
“The government recognized the importance of this technique and have provided what’s called volume-based funding to allow us to operate on a much larger number than most centres.”
My own experience is a vivid illustration of the relief DBS can bring to some Parkinson’s patients.
Holes in my head
I waited a year or so before agreeing to undergo DBS. I had been told I was a good candidate (pending further testing) but needed to steel my courage. When I gave the thumbs-up, it took another year before I was ready for surgery.
I entered Toronto Western Hospital on Sept. 30, 2022 with an idea of what was going to happen, but no real appreciation of what it would feel or sound like.
I knew at some point before the end of the day someone was going to drill a hole in my head. At least one hole. Maybe two.
I was forewarned by reliable parties that the sound of that drilling would be akin to an airplane taking off. More like Concorde taking off inside my head!
Before surgery I had a metal structure bolted to my skull, not unlike the square lightshade at the top of a lamppost.

This was meant to hold my head steady during the MRI scan and throughout the more delicate procedure of skewering my brain without damaging the useful bits.
In the surgical suite there was a bustle of activity as half a dozen surgeons and nursing staff prepared for the procedure. My head frame was bolted to the surgical table, and plastic sheets were draped over me to create an antiseptic site for the skull opening.
The drilling of two nickel-sized holes in my skull was every bit as loud as I had been warned. But no pain, just a feeling of pressure.
In the back of the suite, a cluster of medical IT specialists sat in front of computer screens ready to track and to provide feedback and directions as to where the probes needed to go in my brain.
I know all of this because I was awake — wide awake — for the duration of the six-hour long surgery. I have spent plenty of time around hospitals, both as a patient and as the child of a hospital worker. I’ve covered many medical stories as a reporter. So rather than fear, the prospect of this procedure filled me with curiosity. How would it feel? What would it change? Would it work?
A strange experience indeed
The surgical suite hummed with the normal hubbub of a workplace. The surgeons and I kept up an amiable conversation as I asked questions about what was happening. In the background, a steady staccato, like the noise of a Geiger counter, attested to the continuing activity in my brain.
Clicks coming through a loudspeaker amplified the activity of each busy cell.
It was a strange experience to have someone rooting through your brain.

There was no feeling to it as the brain has no pain sensors. But as the probes slid into place, there were tell-tale signs that gave away what was happening — most commonly a tingling feeling in an arm or leg — as the surgeons carefully threaded the electrodes through my brain to reach the basal ganglia.
Along the way they asked me whether I could recite the days of the week, the months of the year backwards skipping every second month, and the progression of prime numbers to the fifth integer.
Once the probes were in place, it was time to install the wiring and other hardware. For this part of the surgery, anesthetic was required and I was put soundly to sleep. Both probes are attached to wires that are threaded through the skull and under the skin behind the ear, down the neck, over the clavicle and finally are plugged into a battery-operated pulse generator — similar to a pacemaker — that sits just under the skin of the chest. While the surgery involves all the usual risks of infection, hemorrhage, stroke and heart attack, side effects are rare.
A shocking conclusion
So, does it work?
Well, you can see the party trick I’ve been boasting about in the video above or by clicking here. You be the judge.
Here is how it works.
Once the electrodes have been implanted in the brain, their ability to deliver the required electrical stimulation is controlled by a pulse transmitter and an adapted cellphone.

The cellphone carries an app that controls the frequency of the electrical stimulation of the basal ganglia. The stimulator is set to discharge regular electrical pulses day and night that miraculously override or disrupt the scrambled neural instructions that are a Parkinson’s hallmark.
Suddenly I am able to walk normally. There are no tremors. The annoying signs of dyskinesia — those involuntary movements I described above — seem to disappear.
WATCH | In September 2022, before undergoing DBS, Harry Forestell described to his audiences what he was undertaking:
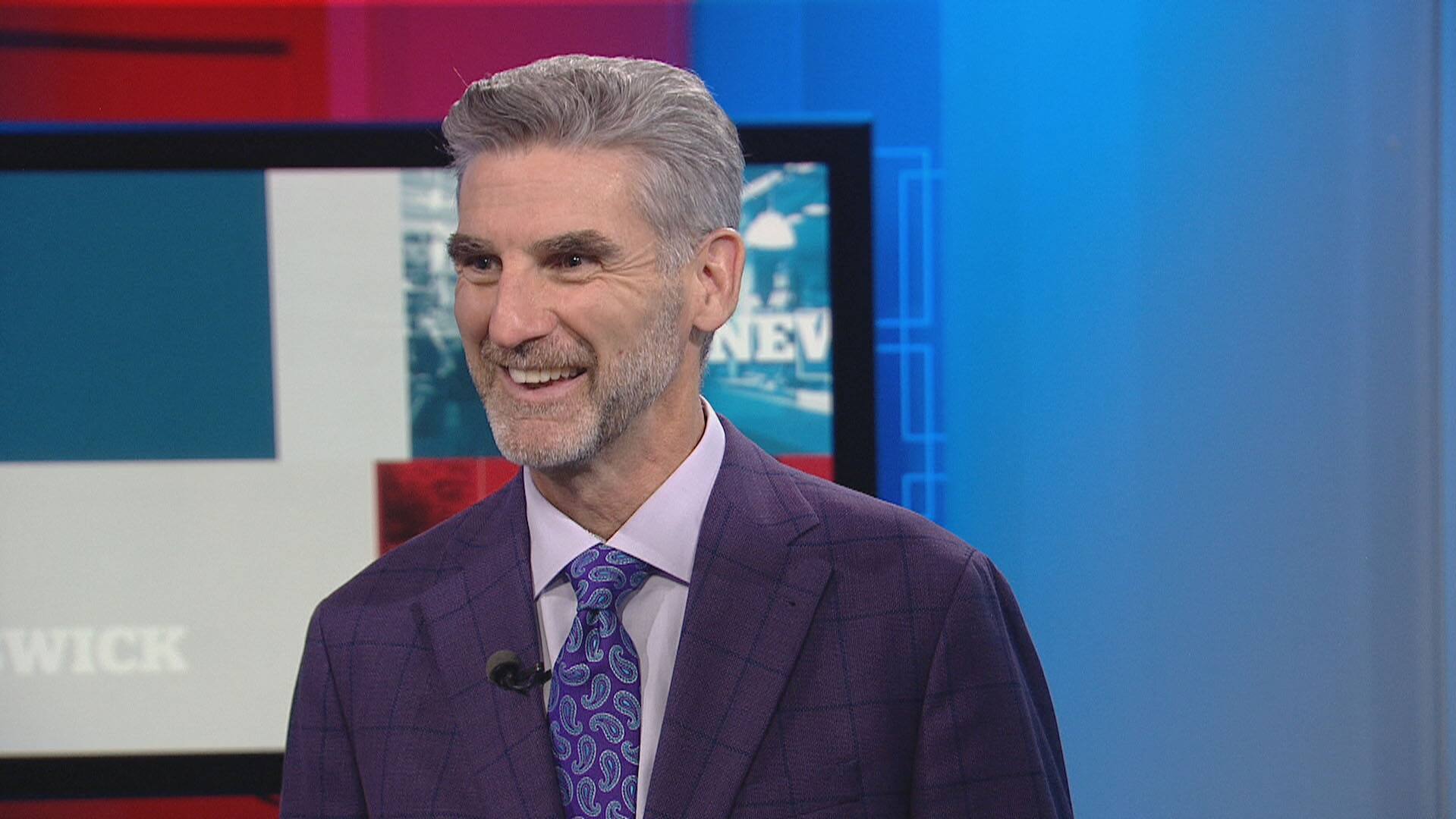
Harry Forestell opens up about the next stage in his treatment for Parkinson’s
The host of CBC New Brunswick News at 6 speaks with Rachel Cave about how deep brain stimulation is expected to help him deal with his Parkinson’s disease diagnosis.
Regaining control of motor functions is nothing short of a miracle, but it will not work for every Parkinson’s patient. Those with other conditions are not suited for DBS. It alleviates motor symptoms most successfully among those who respond well to levodopa. Where it is successful in those cases, it means a decrease in that drug and its side effects.
I have been able to cut my medication in half and I recently returned to work after four months away. I sleep soundly and, while I still tire easily, my mood has brightened.
Parkinson’s disease will continue to dog my life. DBS may allow me another 10 or 15 years without disabling tremors, though they will probably return at some point as they continue to grow in intensity. There are other insidious effects of Parkinson’s that are not affected by DBS.
But for the time being, it is as though the disease is caged.
On a leash.
I can hear it barking, but for now at least, it can’t bite me.
Do you have a compelling personal story that can bring understanding or help others? Here’s more info on how to pitch to us.
